The diet that will make you smile
Nutrition research is hard. We, humans, are terrible at giving an accurate recall of our dietary practices. Are you like me and have a hard time remembering lunch from a couple days ago?
And while we do have large population data on the Mediterranean diet and this carries weight because of the number of people studied (Prinelli et al., 2015), up until 2017 we didn’t have the gold standard randomized control trial (RCT) on diet and mood. Then, there came the SMILES trial.
The SMILES trial is exciting in large part because it gave us the first RCT on the subject, but there are some super fascinating learnings from it I wanted to highlight.
First, what did they look at in the trial?
The main question the researchers were trying to answer was if improving diet would improve mental health?
To study this, they created two groups. Group I received dietary support on the Mediterranean diet and Group II just received social support.
To be included in the study, participants had to be adults, have poor intake of fiber, lean protein and veggies. The group also included people on antidepressants and/or in psychotherapy and depression and anxiety were measured with standardized questionnaires.
What was the Mediterranean diet support?
Seven dietary support sessions with a dietician
Dietary history
Food hampers with Med diet staples like olive oil and recipes
What did they find?
In the Med diet group, they found participants had a significantly greater improvement in their depression rating. They also showed a decrease in anxiety and 32% of the group went into remission (Jacka et al., 2017).
What can we take home from these findings?
There are two points worth highlighting here. One, is the guidance in how to deliver dietary changes and second, what it took to achieve significant change in symptoms.
First, participants had a significant amount of face time with the dietician. Over 3 months, they met 7 times to discuss the principles of the diet and also create personalized goals and recommendations. In practice, this means we need multiple touch points to achieve dietary changes. Be it through health coaching as part of membership or group classes like, Dr and the Chef, this is something I’ve taken to heart in creating a practice experience.
On the other hand, many times diet change can feel overwhelming. All or nothing thinking can really get in the way. Or “clean” foods vs “dirty” foods. However, the types of changes they saw in the trial could feel really achievable. They looked like:
Whole grain intake increased by about 1.2 servings
Using slightly more olive oil
Servings of legumes increased by about 1.5
Fish intake increased by 1.12 servings per week
And significant reduction in servings of unhealthful food (the average decrease was 21.76 servings/week)
I think food and nutrition continues to be a missing piece of our mental health (even general health) discussion and while it may not be a silver bullet or the only intervention, it definitely needs to take its seat at the table (pun majorly intended).
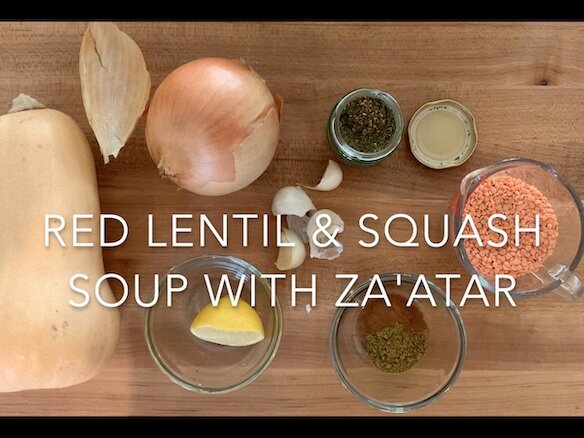
And don’t worry, I’ve got your covered in terms of recipes:
References:
Jacka, F. N., O’Neil, A., Opie, R., Itsiopoulos, C., Cotton, S., Mohebbi, M., Castle, D., Dash, S., Mihalopoulos, C., Chatterton, M. L., Brazionis, L., Dean, O. M., Hodge, A. M., & Berk, M. (2017). A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine, 15. https://doi.org/10.1186/s12916-017-0791-y
Prinelli, F., Yannakoulia, M., Anastasiou, C. A., Adorni, F., Di Santo, S. G., Musicco, M., Scarmeas, N., & Correa Leite, M. L. (2015). Mediterranean diet and other lifestyle factors in relation to 20-year all-cause mortality: A cohort study in an Italian population. The British Journal of Nutrition, 113(6), 1003–1011. https://doi.org/10.1017/S0007114515000318